Donald Hoffman interview on spacetime, consciousness, and how biological fitness conceals reality. We discuss Nima Arkani-Hamed’s Amplituhedron, decorated permutations, evolution, and the unlimited intelligence.
The Amplituhedron is a static, monolithic, geometric object with many dimensions. Its volume codes for amplitudes of particle interactions & its structure codes for locality and unitarity. Decorated permutations are the deepest core from which the Amplituhedron gets its structure. There are no dynamics, they are monoliths as in 2001: A Space Odyssey.
Background.
0:00 Highlights.
6:55 The specific limits of evolution by natural selection.
10:50 Don’s born in a San Antonio Army hospital in 1955 (and his parents’ background)
14:44 As a teenager big question he wanted answered, “Are we just machines?“
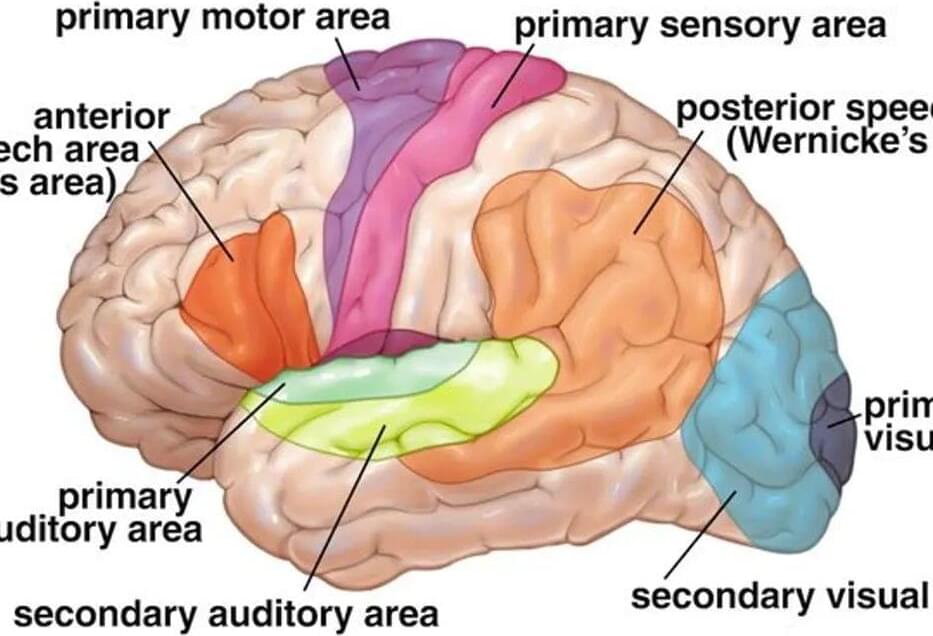
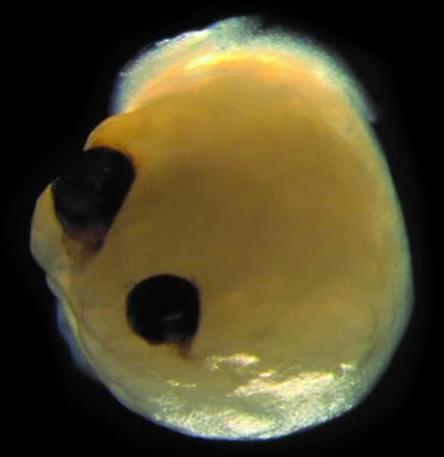
17:23 Don’s early work as a vision researcher; visual systems construct.
20:43 Carlos’s 3-part series on Fitness-Beats-Truth Theorem.
Fitness-Beats-Truth Theorem.
22:29 Clarifications on FBT: Game theory simulations & math proofs.
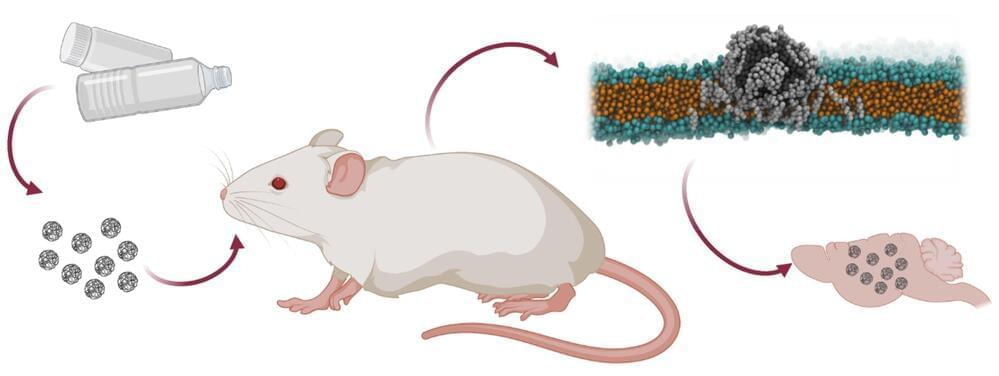
24:20 What does he mean I can’t see reality? Fitness payoff functions don’t know about the truth… 28:23 Evolution shapes sensory systems to guide adaptive behavior… consider the virtual reality headset 32:45 FBT doesn’t include costs for extra bits of information processing 34:40 Joscha Bach’s “There are no colors in the universe”… though even light itself isn’t fundamental! 36:36 Map-territory relationship 40:27 Infinite regress, Godel’s Incompleteness Theorem 42:27 Erik Hoel’s causal emergence theory 45:40 Don’s take on causality: there are no causal powers within spacetime What’s Beyond Spacetime? 50:50 Nima Arkani-Hamed’s Amplituhedron 53:00 What percentage of physicists would agree spacetime is doomed? 56:00 Amplituhedron a static, monolithic, geometric object with many dimensions… 59:23 Ties to holographic principle, Ads-CFT correspondence 1:03:13 Quantum error correction 1:05:23 James Gates’ adinkra animations linking electromagnetism & electron-like objects The Unlimited Intelligence 1:08:30 Does Don still meditate 3 hours every day? 1:11:30 “We’re here for the ride…” 1:12:27 All my theories are trivial, there’s an unlimited intelligence that transcends 1:14:00 Carlos meanders on meditation 1:15:50 “You can’t know the truth, but you can be the truth” 1:17:43 Explore-Exploit Tradeoff (foraging strategy) 1:19:15 “You’re absolutely knocking on the right doors here”… our 4D spacetime for some reason essential for consciousness 1:21:10 Why this world, with these symbols, this interface? 1:22:20 “My guess, one of the cheaper headsets” Conscious Realism 1:24:40 Precise, mathematical model of consciousness… the end of Cantor’s infinities 1:28:30 Fusions of Consciousness paper… bridges between interactions of conscious agents/Markovian dynamics → decorated permutations → the Amplituhedron → spacetime 1:35:20 In a meta way, did Don choose the highest fitness path for his career? 1:39:10 “Don’t believe my theory, not the final word” 1:41:00 Where to find more of Don’s work 🚩Links to Donald Hoffman & More 🚩 “Do we see reality as it is?” (Ted Talk 2015) • Do we see reality…
“Symmetry Does Not Entail Veridicality” lecture (Hoffman 2017)
• Don Hoffman — “Sy…