A new method for medicine.
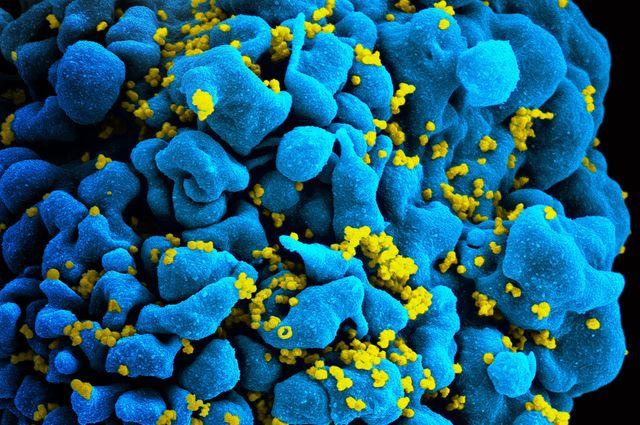
Imagine a cross between one of those multi-color retractable pens and an epi-pen. But instead of colors, the device would have different medications. Now combine this with a tiny, droplet-sized sweatshop full of obedient single-celled organisms genetically engineered to produce those medications, and you’ve got what a team from MIT just published in Nature Communications: A new project, with funding from DARPA, that has demonstrated the ability to synthesize multiple medications on-demand and as-needed using yeast. The discovery could soon revolutionize our ability to deliver medicine after natural disasters or to remote locations.
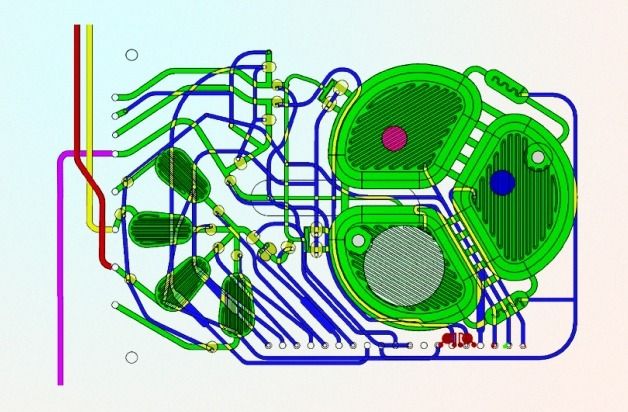
Let’s stick with the metaphor of an epi-pen. First, the user presses the actuator, which mixes a chemical trigger into a culture of engineered Pichia pastoris cells. Upon exposure to certain chemical triggers, the cells are programmed to produce a protein: in the report, the team used estrogen β-estradiol, which caused the cells to express recombinant human growth hormone (rHGH), and also methanol, which induced the same culture of yeast to make interferon. By controlling the concentration of the chemical trigger and the population of P. pastoris, the team demonstrated that they could make their device produce a dose of either interferon or rHGH on command. To switch between products, they just pushed another button on the microbioreactor, which flushes out the cell culture with clean, sterile fluid.
“…rapid and switchable production of two biologics from a single yeast strain as specified by the operator.” –Lu, Ram et al